B-Type Natriuretic Peptide (BNP) Test: Normal Range, Heart Failure Insights & Analysis

I. What is a B-Type Natriuretic Peptide (BNP) Test and Why is it Important for Heart Health?
The B-Type Natriuretic Peptide (BNP) Test measures the level of B-type natriuretic peptide (BNP) in your blood. BNP is a hormone produced by the heart ventricles (lower chambers) in response to the stretching of the heart muscle due to increased blood volume and pressure. When the heart has to work harder than normal, more BNP is released into the bloodstream.
| Condition | BNP Level (pg/mL) | Clinical Interpretation |
|---|---|---|
| Normal | < 100 | Low likelihood of heart failure |
| Possible Heart Failure | 100 – 400 | Needs further evaluation; consider symptoms and additional tests |
| Likely Heart Failure | > 400 | Strong indication of heart failure, requires medical assessment |
The B-type natriuretic peptide (BNP) test is a blood test that has become an important tool for assessing heart function and diagnosing heart failure. When it comes to heart health, early detection and monitoring of potential problems are very important for proper management. This article will explore what a BNP test is, why it’s important, and how it can help manage heart health.
A. Understanding B-Type Natriuretic Peptide and Its Role in Heart Function
1. What is a B-Type Natriuretic Peptide (BNP) Test?
The B-Type Natriuretic Peptide (BNP) test measures the amount of BNP in your blood. BNP is a hormone released by the heart’s ventricles when they stretch due to increased blood volume or pressure. Higher BNP levels indicate that the heart is working harder than usual.
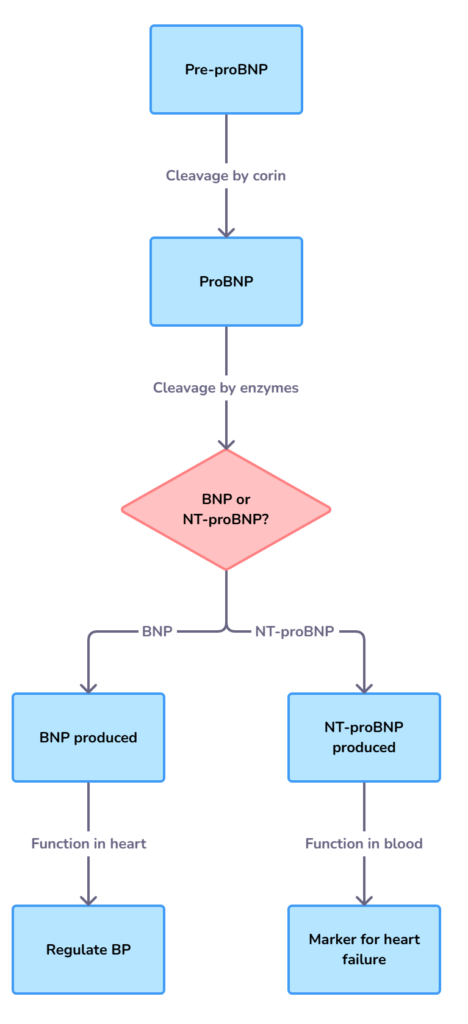
2. How BNP is produced:
- Pre-proBNP: The heart initially produces pre-proBNP.
- ProBNP: Pre-proBNP is then converted to proBNP, which has 108 amino acids.
- BNP and NT-proBNP: ProBNP is further broken down into two substances:
- BNP (B-type natriuretic peptide): a 32-amino acid active hormone
- NT-proBNP (N-terminal pro-B-type natriuretic peptide): a 76-amino acid inactive fragment.
3. What does BNP do?
BNP is a biologically active molecule that has several important functions:
- It helps the body get rid of excess salt and water through the kidneys, known as Natriuresis.
- It causes blood vessels to relax and widen, known as Vasodilation.
- It helps the body to remove excess fluid by increased urination, known as Diuresis.
These actions help reduce the workload on the heart and improve heart function.
B. How B-Type Natriuretic Peptide (BNP) Test Help Detect and Monitor Heart Failure
The BNP test is primarily used to diagnose and manage heart failure (HF). It is particularly useful in patients experiencing acute dyspnea (shortness of breath), which could be due to heart failure or other lung conditions.
1. Diagnosing Heart Failure:
- Early Detection: The BNP test can help detect heart failure even when symptoms are not clear. This is particularly valuable because heart failure symptoms can be similar to other conditions.
- Differentiating Causes of Dyspnea: It helps doctors distinguish between breathing problems caused by heart failure and those caused by lung issues.
2. Monitoring Heart Failure:
- Assessing Severity: BNP levels generally correlate with the severity of heart failure. Higher BNP levels usually indicate more severe heart dysfunction.
- Tracking Treatment Effectiveness: Serial BNP measurements help doctors monitor how well heart failure treatments are working. A decrease in BNP levels often indicates that the treatment is effective.
- Prognosis: BNP levels can help predict the risk of future heart failure events and mortality. Patients with elevated levels, even without acute symptoms, have a poorer prognosis.
3. Risk Stratification:
- Identifying High-Risk Patients: The BNP test can help identify patients at high risk of developing heart failure. This may allow doctors to implement preventive strategies.
- Guiding Treatment Strategies: In clinical trials, BNP levels help identify patients at a higher risk of cardiovascular events, enabling better-targeted therapies.
4. In Adult Congenital Heart Disease
- Prognostic Value: BNP levels can help assess risk of adverse events in patients with adult congenital heart disease.
- Routine Surveillance: Regular BNP testing is recommended as a routine part of follow-up care in patients with adult congenital heart disease.
5. Other conditions
- Cardiac Sarcoidosis: BNP can also predict adverse events in patients with cardiac sarcoidosis {an inflammatory condition where small clumps of immune cells (granulomas) form in the heart, potentially disrupting its electrical system and function}, and may be useful in guiding immunomodulating therapies.
- COVID-19: BNP can be used to assess the prognosis of COVID-19 infections.
II. How the BNP Test Works
A BNP test is a simple blood test that can be performed in a hospital, clinic, or primary care setting. It involves a standard blood draw from a vein in your arm. The blood sample is then sent to a laboratory for analysis, and the results are usually available within a short time.
A. Interpreting BNP Test Results
- Normal Range: Normal BNP levels vary depending on age, sex and specific clinical situation, and the presence of conditions like kidney disease, but generally, a BNP level below 100 pg/mL is considered normal.
- Elevated Levels: Higher BNP levels may indicate heart failure, but they can also be due to other conditions, including kidney disease, high blood pressure, and lung disease.
- Age and Sex: BNP levels tend to be higher in older people and women.
B. Factors that can influence BNP Levels:
| Factors that can Increase BNP Levels | Factors that can Decrease BNP Levels |
|---|---|
| Increasing age | Obesity |
| Female sex | Some medications (e.g., beta-blockers) |
| Kidney disease | |
| High blood pressure | |
| Lung disease | |
| Hyperthyroidism | |
| Other conditions like Cushing’s or Conn’s syndrome |
It is essential to consider the patient’s overall clinical picture when interpreting BNP test results.
C. Differences Between BNP and NT-proBNP Tests
Both BNP and N-terminal pro-BNP (NT-proBNP) are measured to assess heart health, but they are different substances.
| Feature | BNP | NT-proBNP |
|---|---|---|
| Type | Biologically active hormone | Inactive fragment |
| Half-life | Shorter (about 20 minutes) | Longer (about 120 minutes) |
| Metabolism | Metabolized by enzymes and kidney to some degree | Primarily cleared by the kidneys and other organs |
| Stability | More susceptible to degradation during blood sampling and storage | More stable |
| Use in Testing | Often used in the emergency diagnosis of acute heart failure | Often used in both acute and chronic settings and in primary care |
| Cut-off Levels | 100 pg/mL is a common cut off point in acute setting | Age and clinical context dependent cut offs |
Key Differences to Remember:
- Activity: BNP is biologically active, while NT-proBNP is inactive.
- Half-life: NT-proBNP has a longer half-life than BNP, making it more stable and less prone to degradation before testing.
- Cut-off Values: NT-proBNP has different cut-off values from BNP, depending on the age, patient setting, and the clinical question being addressed.
Due to its increased stability and longer half-life, NT-proBNP is often preferred for testing when measuring changes in heart failure over time, and is often used in primary care and ambulatory settings. However, both tests are useful for evaluating heart health.
Study Highlight: The study by Maisel AS et al. (2002) published in the New England Journal of Medicine demonstrated that rapid measurement of BNP can significantly improve the diagnosis of heart failure in emergency settings. This landmark study highlighted the importance of BNP as a diagnostic tool in acute care.
III. Preparing for Your BNP Blood Test: A Simple Guide
The B-type natriuretic peptide (BNP) blood test is a common and straightforward procedure that helps healthcare professionals assess your heart health. Knowing how to prepare for the test and what to expect can make the process easier and more comfortable. This section will guide you through everything you need to know before, during, and after your BNP test.
A. How to Prepare for a BNP Blood Test
Fortunately, preparing for a BNP blood test is very simple. Unlike some other medical tests, there are generally no strict rules or requirements. Here’s a breakdown of what you need to know:
- No Fasting Required: You do not need to fast before your BNP test. You can eat and drink normally. This makes the test very convenient as it can be done at any time of the day without specific dietary restrictions.
- Medication: You can usually continue to take your regular medications unless your doctor tells you otherwise. If you have any concerns about your medications, it’s best to consult your healthcare provider beforehand.
- Hydration: Staying hydrated is generally a good idea for any blood test, but it is not a specific requirement for the BNP test. Drinking a normal amount of water is sufficient.
- Comfort: Wear comfortable clothing that allows easy access to your arm. This will make the blood draw easier for the healthcare professional and more comfortable for you.
Summary: The key to preparing for a BNP test is to simply maintain your normal daily routine, unless your doctor has provided specific instructions.
B. Steps to Take Before Your BNP Test
Although the BNP test itself requires minimal preparation, you should consider the following steps:
- Consult Your Doctor: If you have any specific concerns or questions, it’s always a good idea to discuss them with your doctor. They will provide personalised guidance based on your health condition and circumstances.
- Know Your Medications: Be aware of all the medications you are currently taking, including any over-the-counter drugs or supplements. This information can be useful to the healthcare provider.
- Prepare Questions: If you have any concerns or doubts about the procedure or why the test is being done, write down your questions and bring them with you to the appointment.
- Inform about allergies: Let your healthcare provider know if you have any allergies, especially to latex or adhesive tape.
By taking these steps, you will be well-prepared for your BNP test and can ensure the process goes as smoothly as possible.
C. What to Expect During the Blood Sample Collection
The blood sample collection for a BNP test is a routine procedure, typically completed in a few minutes. Here’s what you can expect during the process:
- Identification: The healthcare professional will begin by confirming your identity, usually by asking your name and date of birth. This is a standard safety precaution to ensure the correct sample is taken.
- Vein Selection: The healthcare professional will choose a suitable vein, usually in your arm. They may ask you to make a fist to make your veins more visible.
- Cleaning: The area around the selected vein will be cleaned with an antiseptic wipe. This step is crucial to prevent infection.
- Needle Insertion: A needle will be carefully inserted into your vein. You may feel a small prick or sting, but this sensation is usually brief.
- Blood Collection: Once the needle is in place, a small amount of blood is drawn into a tube attached to the needle. The tube will usually be a lavender top (EDTA) tube for BNP. For NT-proBNP, a red/black top (serum gel) tube is used.
- Needle Removal: After the required amount of blood has been collected, the needle will be removed. A cotton ball or gauze pad will be placed over the insertion site, and a bandage might be applied to help stop any bleeding.
- Sample Processing: The blood sample will then be sent to a laboratory for analysis. For BNP testing, the plasma is often separated and frozen immediately.
The whole process of collecting the blood sample usually takes just a few minutes. You may experience slight discomfort or a small bruise after the procedure, but these are usually very mild and temporary.
D. After Your BNP Blood Test
After the blood sample has been taken, here are a few things to keep in mind:
- Bandage: Keep the bandage in place for a few hours to prevent bleeding.
- Bruising: Some people may develop a small bruise at the site of the needle insertion. This is normal and will usually fade away within a few days.
- Discomfort: If you experience any unusual pain or swelling, contact your healthcare provider.
- Results: Your healthcare professional will inform you about how and when you will receive the results. They will also discuss the implications of the results and the next steps in your treatment plan.
E. Key Takeaways
- Fasting: Not required for the BNP test.
- Medications: Continue to take your regular medications unless instructed otherwise.
- Procedure: A quick and simple blood draw, usually from your arm.
- Aftercare: Minor bruising or discomfort at the injection site is normal.
- Results: Your healthcare provider will discuss the results and any necessary follow-up actions with you.
By understanding these simple steps, you can approach your BNP blood test with confidence and ease. If you have any further questions or concerns, don’t hesitate to discuss them with your doctor.
IV. Decoding BNP Test Results: What Do the Numbers Mean?
The B-type natriuretic peptide (BNP) blood test is a valuable tool for assessing heart health, particularly in the context of heart failure (HF). However, understanding what the results mean can be confusing. This section will help you interpret your BNP test results by explaining normal levels, what high levels may indicate, and other factors that can affect the results.
A. Understanding Normal BNP and NT-proBNP Levels
BNP and NT-proBNP are both substances produced by the heart in response to stress, and they are used as markers for diagnosing and managing heart failure. It’s important to know that normal ranges vary, and they are not absolute. What’s considered normal can depend on factors like age, sex, and individual health conditions.
- BNP (B-type natriuretic peptide): Generally, a BNP level below 100 pg/mL is considered normal and indicates a low likelihood of heart failure. However, this cut-off is primarily used in the acute setting.
- NT-proBNP (N-terminal pro-B-type natriuretic peptide): Normal levels for NT-proBNP are more variable and often increase with age, so age-related thresholds are recommended. For example, a cut-off of <300 pg/mL can be used to rule out heart failure, but higher cut-offs are more suitable for ‘ruling in’ HF:
- < 50 years: > 450 pg/mL
- 50-75 years: > 900 pg/mL
- 75 years: > 1800 pg/mL
- A level less than 125 pg/mL may indicate that heart failure is unlikely, in the non-acute setting.
Note: Women tend to have higher levels of NT-proBNP than men.
Summary of typical cut-off levels for BNP and NT-proBNP:
| Biomarker | Typical ‘Rule-Out’ Threshold | Typical ‘Rule-In’ Thresholds | Notes |
|---|---|---|---|
| BNP | <100 pg/mL | >400 pg/mL | Primarily used in acute settings |
| NT-proBNP | <300 pg/mL | >450 pg/mL (<50 yrs), >900 pg/mL (50-75 yrs), >1800 pg/mL (>75 yrs) | Age-dependent thresholds often used, used in acute settings |
| NT-proBNP | <125 pg/mL | May indicate HF is unlikely in non-acute settings |
B. Interpreting High BNP Levels: Signs of Heart Failure?
Elevated BNP or NT-proBNP levels often suggest that the heart is under stress. Higher levels generally indicate a greater risk of adverse outcomes. Here’s a breakdown of what elevated levels might mean:
- Heart Failure: High levels are commonly associated with heart failure. When the heart muscle is weakened or strained, it releases more BNP and NT-proBNP. The level of elevation can reflect the severity of the heart failure.
- Other Cardiac Issues: Elevated levels can also be seen in conditions such as:
- Left ventricular dysfunction: Both systolic and diastolic dysfunction can lead to higher BNP levels.
- Valvular heart disease.
- Atrial fibrillation.
- Myocardial infarction (heart attack), although patients with acute myocardial infarction were excluded from some studies.
- Congenital heart disease: BNP levels are used for routine surveillance of patients with congenital heart disease.
- Cardiac sarcoidosis: Higher BNP levels in patients with cardiac sarcoidosis are associated with poor outcomes.
- Risk Indicator: Even if heart failure isn’t diagnosed, elevated BNP levels can indicate an increased risk of future cardiac events, including hospitalisation and death. A study by York et al. published in Journal of the American College of Cardiology found that BNP was the strongest predictor of death in patients both with and without heart failure.
Note: An elevated BNP or NT-proBNP result doesn’t always mean you have heart failure. Other factors need to be considered.
C. Factors That Can Affect BNP Test Results
Several factors can influence BNP and NT-proBNP levels, potentially leading to both false positives and false negatives. It’s crucial to consider these factors when interpreting your test results:
- Age: BNP and NT-proBNP levels naturally increase with age, especially in older individuals. Therefore, age-adjusted thresholds are more accurate, particularly for NT-proBNP.
- Sex: Women generally have higher BNP and NT-proBNP levels than men.
- Kidney Disease: Patients with kidney disease often have higher levels of BNP and NT-proBNP, regardless of whether they have heart failure. This is because the kidneys play a role in clearing these peptides from the blood.
- Obesity: Obesity is associated with lower-than-expected BNP and NT-proBNP levels. This may be due to increased clearance of the peptides or other unknown mechanisms.
- Body Mass Index (BMI): A higher BMI is often associated with lower BNP levels, regardless of heart failure status.
- Other Conditions: Conditions like lung disease, infections, and inflammation can also lead to elevated levels. For example, patients with lung conditions like COPD can also have elevated BNP.
- Medications: Certain medications, such as diuretics, may influence BNP levels.
- Time of Day: Some studies suggest that BNP levels may vary throughout the day.
- Assay Variability: The way the test is measured can also have some minor variations. Intra-assay precision can vary.
Given these factors, it’s important to have a comprehensive medical evaluation and not rely solely on BNP or NT-proBNP results for diagnosis.
Key Takeaways
- Normal Ranges: BNP <100 pg/mL and NT-proBNP levels vary by age, with higher thresholds used to ‘rule in’ HF, and lower thresholds used to ‘rule out’ HF.
- Elevated Levels: May indicate heart failure, but other cardiac and non-cardiac conditions can also raise BNP and NT-proBNP.
- Influencing Factors: Age, sex, kidney disease, obesity, and other health issues can affect BNP and NT-proBNP levels, which means the values must be interpreted with caution.
- Individualized Interpretation: It is important to interpret BNP and NT-proBNP levels in the context of a patient’s individual circumstances, and consider other relevant factors.
By understanding these points, you can have a more informed conversation with your healthcare provider about your BNP test results.
V. When Should You Get a BNP or NT-proBNP Test?
The B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) tests are valuable for assessing heart health, particularly in diagnosing and managing heart failure (HF). But when exactly should you consider getting one of these tests? This section will explore common symptoms that might prompt a BNP test and the risk factors that make testing more appropriate.
A. Common Symptoms That May Prompt a BNP Test
The primary reason for getting a BNP or NT-proBNP test is to investigate symptoms that suggest your heart might not be working as well as it should. These symptoms can vary, but here are some of the most common ones:
- Shortness of Breath (Dyspnea): This is one of the most frequent reasons for a BNP test, especially when it occurs at rest or with minimal activity. It can be a sign that your heart is not pumping enough blood to meet your body’s needs, causing fluid to back up into your lungs.
- Fatigue: Feeling unusually tired or weak, even after adequate rest, can be a sign of heart problems. This fatigue can result from reduced blood flow to your muscles and organs.
- Swelling (Edema): Swelling in your legs, ankles, or feet can be a sign of fluid retention due to heart failure. This happens because a weakened heart is not effectively pumping blood, leading to fluid accumulation in the body.
- Persistent Coughing or Wheezing: This symptom may be associated with fluid build-up in the lungs due to heart failure.
- Rapid or Irregular Heartbeat: If you experience palpitations, a racing heart, or an irregular pulse, it might be a sign of underlying heart issues that a BNP test can help investigate.
- Dizziness or Lightheadedness: These symptoms can occur if your heart is not pumping enough blood to the brain.
- Unexplained Breathlessness: If you experience breathlessness with no clear explanation (e.g., lung disease), a BNP or NT-proBNP test can help determine if heart failure is the underlying cause.
It’s important to note that these symptoms are not specific to heart failure and can be caused by other conditions. Therefore, a BNP or NT-proBNP test is often used alongside other tests to help make an accurate diagnosis.
When to Seek Immediate Medical Attention: If you experience sudden or severe shortness of breath, chest pain, or fainting, seek immediate medical attention as these may be signs of a serious heart problem.
B. Risk Factors for Heart Failure and BNP Testing
Certain risk factors can make you more likely to develop heart failure, and therefore, more likely to benefit from a BNP or NT-proBNP test. These risk factors include:
- High Blood Pressure (Hypertension): Over time, high blood pressure can strain the heart, increasing the risk of heart failure.
- Coronary Artery Disease (CAD): This condition, where the arteries supplying the heart become narrowed or blocked, can lead to heart damage and failure.
- Diabetes: High blood sugar levels can damage the heart muscle and blood vessels, increasing the risk of heart failure.
- Obesity: Carrying excess weight can put extra strain on the heart, leading to heart failure. A higher body mass index (BMI) is associated with lower BNP levels but can still increase your risk of heart failure.
- Family History of Heart Disease: If you have a family history of heart disease, you may be at higher risk.
- Advanced Age: The risk of heart failure increases with age.
- Valvular Heart Disease: Problems with the heart valves can force the heart to work harder and may lead to heart failure.
- Previous Heart Attack (Myocardial Infarction): A heart attack can damage the heart muscle, leading to heart failure.
- Kidney Disease: Impaired kidney function can increase the risk of heart failure and may also affect the levels of BNP and NT-proBNP.
- Congenital Heart Defects: People born with heart defects are at increased risk of heart failure.
- History of Atrial Fibrillation: Having an irregular heart rhythm can increase the risk of developing heart failure.
If you have one or more of these risk factors, it’s important to discuss with your healthcare provider whether a BNP or NT-proBNP test is appropriate for you, particularly if you also have any of the symptoms described above.
C. BNP and NT-proBNP Testing in Specific Settings
- Emergency Department (Acute Dyspnea): In the emergency setting, BNP and NT-proBNP tests are crucial for rapidly distinguishing between heart failure and other causes of shortness of breath. A BNP level of 100 pg/mL or less can rule out heart failure as the cause of acute dyspnea, while higher values are associated with heart failure. For NT-proBNP, age-adjusted cut-offs are used to diagnose HF in an acute setting, with values greater than 450 pg/mL for those under 50, greater than 900 pg/mL for 50-75 years of age, and greater than 1800 pg/mL for those over 75.
- Outpatient Setting: In ambulatory care, BNP and NT-proBNP tests can help diagnose heart failure in patients with new or worsening symptoms. Lower thresholds are often used in this setting to avoid false negative results, as symptoms are usually less severe. An NT-proBNP level of less than 125 pg/mL can suggest heart failure is unlikely in non-acute settings.
- Monitoring Heart Failure: For those already diagnosed with heart failure, BNP and NT-proBNP tests can help monitor the condition and the effectiveness of treatment. Changes in these levels over time can indicate whether the condition is improving, worsening, or stable.
D. When is BNP/NT-proBNP Testing Not Recommended?
While BNP and NT-proBNP tests are useful in many situations, they may not be appropriate for everyone. For example:
- Asymptomatic Individuals: Routine screening with BNP or NT-proBNP is not generally recommended for people who don’t have symptoms of heart failure, although it may be useful in those at high risk.
- Known Non-Cardiac Causes: If your shortness of breath is clearly due to a non-cardiac condition, like a lung disease or trauma, a BNP or NT-proBNP test may not be necessary.
Summary
When a BNP or NT-proBNP test may be recommended:
| Symptom/Situation | Rationale |
|---|---|
| Unexplained shortness of breath, fatigue, or edema | To help determine if heart failure may be the cause. |
| Known or suspected heart disease | To assess the severity of heart failure and guide treatment. |
| New onset or worsening of heart failure symptoms | To monitor disease progression and response to treatment. |
| Patients at high risk for heart failure | To identify subclinical dysfunction and potentially prevent disease progression. |
| Differential diagnosis of dyspnea in an acute setting | To quickly distinguish cardiac from non-cardiac causes of breathlessness. |
E. Key Takeaways
- Common Symptoms: Shortness of breath, fatigue, swelling, and irregular heartbeat can be signs of heart issues and may warrant BNP/NT-proBNP testing.
- Risk Factors: High blood pressure, diabetes, obesity, and family history of heart disease are significant risk factors that may increase the need for BNP testing.
- Emergency Setting: BNP and NT-proBNP are valuable tools in the emergency department for diagnosing heart failure.
- Outpatient Setting: Testing can be useful in diagnosing heart failure and monitoring the disease in those with chronic conditions.
- Not for Everyone: Testing is not typically recommended for asymptomatic individuals with no risk factors.
This information should help you understand when to consider a BNP or NT-proBNP test. Always consult with your healthcare provider to determine the most appropriate course of action for your specific situation.
VI. How Do Doctors Use BNP Tests to Diagnose Heart Failure?
B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) tests are vital tools for doctors in the diagnosis and management of heart failure (HF). These tests measure the levels of these substances in the blood, which are released by the heart in response to stress and strain. This section explains how doctors use BNP tests to diagnose heart failure, focusing on their role in diagnosis and how they are used alongside other diagnostic tools.
A. The Role of BNP in Heart Failure Diagnosis
- What are BNP and NT-proBNP? BNP and NT-proBNP are neurohormones produced by the heart in response to ventricular volume expansion and pressure overload. When the heart is strained, such as in heart failure, it releases more of these peptides. BNP is the biologically active hormone, while NT-proBNP is an inactive fragment of the prohormone.
- Why are they useful? Elevated levels of BNP and NT-proBNP in the blood can indicate that the heart is under stress. These peptides act as quantitative markers of HF, reflecting the extent of systolic and diastolic left ventricular dysfunction. They help doctors determine whether a patient’s symptoms are likely due to heart failure or another condition.
- Diagnostic accuracy: BNP and NT-proBNP tests, when used alongside other clinical information, significantly increase diagnostic accuracy. The use of BNP in patients presenting with acute dyspnoea increases the accuracy of clinical evaluation.
- The Breathing Not Properly trial showed that a BNP threshold of 100 pg/mL could differentiate between heart failure and other causes of dyspnoea with high accuracy.
B. Using BNP in Different Clinical Settings
- Acute Dyspnea: In the emergency department, patients often present with shortness of breath, which could be due to various causes. Rapid measurement of BNP can help doctors quickly differentiate heart failure from other causes, such as lung disease.
- A BNP level below 100 pg/mL has a high negative predictive value (NPV), suggesting that heart failure is unlikely.
- Conversely, higher BNP levels, especially above 400 pg/mL, have a good positive predictive value (PPV), indicating a greater likelihood of heart failure.
- For NT-proBNP, age-related cut-offs are preferred: >450 pg/mL for patients under 50, >900 pg/mL for those 50 and older. However, an NT-proBNP concentration <300 pg/mL provides a very high NPV for HF.
- Chronic Heart Failure: For patients with chronic HF, BNP and NT-proBNP tests can be used to assess the severity of the condition and to monitor the effectiveness of treatment.
- Ambulatory Settings: In outpatient settings, these tests are useful for patients with new symptoms suggestive of heart failure. In non-acute settings, an NT-proBNP of <125 pg/mL is considered a rule-out threshold for heart failure.
C. Combining BNP Results with Other Diagnostic Tools
BNP tests are most effective when used in combination with other diagnostic tools and clinical assessments. Here’s how:
- Clinical Evaluation: Doctors will consider your medical history, symptoms, and a physical examination. This includes checking for signs like swelling (oedema), abnormal heart sounds, and breathing difficulties. The clinical diagnosis of heart failure can be challenging, and BNP testing can improve the accuracy.
- Electrocardiogram (ECG): An ECG records the electrical activity of your heart and can help detect abnormalities in heart rhythm and identify prior heart attacks that might have contributed to heart failure.
- Chest X-Ray: This imaging test can show if there is fluid build-up in the lungs (pulmonary congestion) or an enlarged heart, both of which are signs of heart failure.
- Echocardiogram: This ultrasound test provides detailed images of the heart’s structure and function, including the pumping ability of the heart (ejection fraction) and any valve problems. An echocardiogram is often used as a reference standard for comparison with BNP test results.
- Other Blood Tests: Doctors may also order other blood tests to assess kidney function, liver function, and electrolytes, which can also affect heart health.
- The importance of a holistic approach: It is important to note that BNP levels should not be used in isolation to diagnose or exclude heart failure. Clinical interpretation requires understanding the patient’s clinical context, including factors that can influence BNP levels. These include age, sex, kidney function, and other medical conditions.
- For example, natriuretic peptide levels are consistently higher in patients with chronic kidney disease.
- Conversely, patients with obesity may have lower than expected BNP levels.
D. How do doctors interpret BNP results?
- Rule-out and Rule-in: Doctors use BNP results to both “rule out” and “rule in” heart failure. A low BNP or NT-proBNP result, especially in the context of a low pre-test probability, helps rule out heart failure. A high result in combination with other symptoms and risk factors, will strengthen a diagnosis of heart failure.
- Gray Zone: When natriuretic peptide levels fall between the rule-out and rule-in thresholds, doctors may call this the ‘grey zone’. About 20% of patients with acute dyspnea have levels in this range, and about half of them may have heart failure. These patients require further evaluation and testing, such as chest x-rays and echocardiography.
- Individual Patient Trajectories: Doctors may track an individual’s BNP levels over time, especially in patients with chronic heart failure. This approach helps to integrate the results, accounting for different factors. A change of 25-30% from a stable level can indicate a change in clinical status.
E. BNP and NT-proBNP Thresholds
The table below provides an overview of typical BNP and NT-proBNP thresholds used in clinical practice:
| Setting | Marker | Threshold |
|---|---|---|
| Acute Dyspnea (Rule-out) | BNP | < 100 pg/mL |
| Acute Dyspnea (Rule-in) | BNP | > 400 pg/mL |
| Acute Dyspnea (Rule-in, age-related) | NT-proBNP | >450 pg/mL (under 50 years), >900 pg/mL (50 and older) |
| Non-Acute Setting (Rule-out) | NT-proBNP | <125 pg/mL |
| Chronic HF Monitoring | BNP/NT-proBNP | Changes of ≥ 25-30% from baseline indicate change in clinical status |
F. Key Takeaways
- Diagnostic Markers: BNP and NT-proBNP are important biomarkers for diagnosing heart failure, especially in patients with dyspnea.
- Multiple Settings: These tests are useful in emergency departments, outpatient clinics, and for monitoring chronic heart failure.
- Complementary Use: BNP results should be interpreted alongside other clinical information such as patient history, physical exam, ECG, chest x-ray, and echocardiography.
- Thresholds: Specific cutoffs aid in ruling in or ruling out heart failure, but the “grey zone” requires further evaluation.
- Context is Key: Individual patient factors, such as age, sex, kidney function and other co-morbidities, need to be taken into account when interpreting BNP levels.
VII. Can BNP Tests Help Monitor Heart Failure Treatment?
B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) tests are not only useful for diagnosing heart failure (HF), but also play a crucial role in monitoring the effectiveness of treatment and tracking disease progression. This section will explore how doctors use BNP levels to monitor heart failure, what strategies are employed to lower these levels, and how these actions can lead to improved heart health.
A. Using BNP Levels to Track Heart Failure Progress
- Monitoring Treatment Effectiveness: Serial measurements of BNP and NT-proBNP levels can help doctors assess how well a patient is responding to heart failure treatment. If treatment is effective, BNP levels should decrease over time.
- Prognostic Value: BNP and NT-proBNP are among the most powerful prognostic markers in all forms of clinical heart failure, including acute and chronic conditions.
- Both initial BNP values and changes in BNP levels with therapy are strong predictors of short and long-term outcomes.
- A study from the OPTIMIZE-HF registry demonstrated that both admission and discharge BNP levels are important predictors of long term outcomes.
- Predicting Hospital Readmission: Elevated BNP or NT-proBNP levels at the time of hospital discharge are strong indicators of increased risk for future hospital readmission and death. These levels help doctors predict post-discharge prognosis and optimize treatment.
- For instance, a 2023 study published in JCF (Journal of Cardiac Failure) showed that discharge BNP levels are a stronger predictor of six-month mortality in acute heart failure compared to baseline BNP levels.
- Guiding Therapy Adjustments: Some clinicians use BNP levels to guide the adjustment of medications and other therapies. This approach is often referred to as biomarker-guided therapy. The goal is to achieve specific target levels of BNP or NT-proBNP, which may indicate improved heart function and reduced symptoms.
- Understanding Clinical Stability: When natriuretic peptide testing was first introduced, clinicians noted that levels often tracked with clinical stability. However, there can be wide variations in levels among patients with similar symptoms, requiring adjustments to individualise clinical interpretation.
- For example, A study published in Journal of the American College of Cardiology mentions that almost a quarter of patients with chronic symptomatic heart failure may have natriuretic peptide levels in the lower ranges.
- Tracking Individual Patient Trajectories: The most effective clinical strategy involves tracking each patient’s individual natriuretic peptide trajectory while accounting for other factors. Source
B. Strategies to Lower BNP Levels and Improve Heart Health
The primary strategy to lower BNP levels is to manage the underlying heart failure with a combination of lifestyle changes and medical therapies. Here are some key strategies:
- Medications:
- Angiotensin-Converting Enzyme (ACE) inhibitors and Angiotensin Receptor Blockers (ARBs): These medications help to relax blood vessels and reduce the workload on the heart, which can reduce BNP levels.
- Angiotensin Receptor Neprilysin Inhibitors (ARNIs): These medications are shown to reduce NT-proBNP levels by about 30% compared to ACE inhibitors or ARBs. They are particularly useful in patients with reduced ejection fraction.
- Beta-blockers: These help to slow the heart rate and reduce blood pressure, thereby decreasing the workload on the heart and lowering BNP levels over time.
- Diuretics: These medications help the body remove excess fluid and reduce volume overload, thus lowering BNP levels.
- Mineralocorticoid Receptor Antagonists (MRAs): These help reduce fluid retention and are used in combination with other heart failure therapies to lower BNP levels.
- Lifestyle Modifications:
- Dietary Changes: Reducing sodium intake and limiting fluid intake can help reduce fluid retention and ease the workload on the heart.
- Regular Exercise: Moderate exercise, as advised by a healthcare provider, can improve cardiovascular health and reduce BNP levels over time.
- Weight Management: Maintaining a healthy weight can reduce the strain on the heart and help lower BNP levels.
- Smoking Cessation and Alcohol Limitation: These lifestyle changes are essential for cardiovascular health and will support better heart function.
- Device Therapy:
- Implantable Cardioverter Defibrillators (ICDs): These devices can prevent sudden cardiac arrest in high-risk patients, improving overall outcomes.
- Cardiac Resynchronisation Therapy (CRT): This treatment can improve heart function in patients with specific electrical conduction abnormalities, potentially reducing BNP levels.
C. BNP Targets and What They Mean
- No Universal Target: There is no universally agreed-upon target level for BNP or NT-proBNP. Instead, doctors focus on individual patient responses and trends in BNP levels over time.
- Individualised Approach: The focus is on achieving the lowest possible BNP level while maintaining clinical stability. The magnitude of reduction in BNP levels that is associated with clinical benefit may vary between individuals.
- Relative Reductions: Some studies focus on relative reduction in BNP levels over time as treatment goals. For example, a reduction of 30% in NT-proBNP may be targeted during acute heart failure admissions.
- It is important to note that natriuretic peptide levels have intrinsic biological variability (25% for NT-pro-BNP and 40% for BNP), so changes greater than this can indicate a meaningful change in clinical condition.
D. Limitations of BNP-Guided Therapy
While BNP-guided therapy has shown promise, it’s essential to understand its limitations:
- BNP levels don’t always reflect clinical status: BNP concentrations mainly reflect congestion in advanced HF or in decompensated disease, but in chronic stable disease, the main determinant of BNP or NT-proBNP concentrations is transmural wall stress.
- Individual variability: BNP levels can vary widely among patients with the same degree of symptoms or echocardiographic parameters, requiring occasional adjustments to individualize clinical interpretation.
- Confounding Factors: Several factors can influence BNP levels, including age, sex, kidney function, and other medical conditions. These factors should be taken into account when interpreting BNP levels.
- For instance, natriuretic peptide levels are consistently higher in patients with underlying chronic kidney disease.
- Lack of Standardised Protocols: There are no universally agreed-upon protocols for using BNP levels to guide heart failure management.
- Limited data on long-term benefits: While some studies have suggested that therapy-related changes in natriuretic peptide levels correlate with decreased HF hospitalization rates, other studies show that these changes may not correlate with effects on cardiovascular or all-cause mortality.
- Not a standalone measure: It is important to emphasize that BNP levels should not be the sole factor in determining treatment plans. BNP levels should be interpreted along with other clinical data and patient-specific factors.
E. Key Takeaways
- Monitoring Tool: BNP and NT-proBNP tests are valuable for monitoring the progress of heart failure treatment.
- Treatment Effectiveness: A reduction in BNP levels typically indicates that treatment is working, whereas an increase may warrant further investigation and treatment adjustment.
- Prognostic Markers: These tests help in risk stratification and can predict adverse outcomes such as hospital readmission and mortality.
- Individualized Approach: Treatment decisions should be guided by individual patient response, alongside BNP measurements, rather than specific targets.
- Comprehensive Approach: BNP levels are best used as part of a holistic approach to heart failure management, which includes medication, lifestyle changes, and device therapy.
VIII. Are There Any Limitations or Considerations for BNP Testing?
While B-type natriuretic peptide (BNP) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) tests are valuable tools in the diagnosis and management of heart failure (HF), it’s important to be aware of their limitations and the factors that can influence their accuracy. This section will explore these considerations to help you better understand the appropriate use of BNP testing.
A. Factors That May Affect BNP Test Accuracy
Several factors can influence BNP and NT-proBNP levels, leading to potentially misleading results. It is crucial to consider these factors when interpreting test results:
- Age: BNP and NT-proBNP levels tend to increase with age, even in healthy individuals. This means that older adults may have higher BNP levels, which may not necessarily indicate heart failure. For NT-proBNP, age-adjusted thresholds are often used.
- Sex: Studies have shown that women often have higher NT-proBNP levels compared to men. This difference should be considered when interpreting results.
- Obesity: Individuals with obesity may have lower BNP and NT-proBNP levels than expected, potentially leading to false-negative results. This is possibly due to the increased volume of blood, and greater clearance of the peptides in obese individuals.
- Kidney Disease: Patients with chronic kidney disease often have elevated BNP and NT-proBNP levels due to reduced clearance of these peptides by the kidneys. This makes it more challenging to interpret BNP results in patients with kidney issues. In end-stage renal disease, BNP levels can be 10-fold higher than normal ranges.
- Acute Illness: Conditions such as infections, inflammation, and fever can cause a transient increase in BNP and NT-proBNP levels. These increases are due to the body’s stress response rather than heart dysfunction.
- Pulmonary Conditions: Conditions such as pulmonary embolism or pneumonia can also cause elevations in BNP, making it less specific for heart failure diagnosis in such cases.
- Other Cardiac Conditions: Issues such as acute coronary syndrome or valvular heart disease can lead to elevated BNP levels, meaning the tests cannot be used as stand-alone indicators for HF.
- Anemia: Anemia can affect the accuracy of BNP testing, with lower hemoglobin levels correlating with higher BNP levels.
- Medications: Certain medications, such as angiotensin receptor neprilysin inhibitors (ARNIs) can increase BNP levels, but not NT-proBNP levels. This is because BNP is a substrate for neprilysin, an enzyme inhibited by ARNIs, whereas NT-proBNP is not.
- Assay Variability: Different assays for measuring BNP and NT-proBNP may have slight variations in results. It’s important for healthcare providers to be aware of the specific assay used by their local laboratory to ensure accurate interpretations.
B. When Additional Tests May Be Needed Beyond BNP
BNP and NT-proBNP tests are not perfect diagnostic tools and should not be used in isolation. In many cases, further testing may be required to confirm or rule out heart failure.
- “Grey Zone” BNP Levels: When BNP levels fall within an intermediate range (typically between 100-400 pg/mL), it can be challenging to interpret results. Additional testing and clinical evaluation are essential in such cases. About 25% of patients presenting with acute dyspnoea have BNP levels in this grey zone.
- Clinical Assessment: A thorough clinical assessment, including a patient’s medical history, physical examination, and symptoms, is critical to interpret BNP results. BNP levels should always be considered alongside this clinical information, not in isolation.
- Echocardiography: Echocardiography is often needed to assess the structure and function of the heart. This is particularly important for individuals with intermediate BNP levels, or when there’s a suspicion of structural heart disease. Echocardiography can determine the ejection fraction and identify other heart abnormalities.
- A staged approach for ambulatory patients is often used with initial natriuretic peptide screening, followed by echocardiography in patients with elevated values.
- Electrocardiogram (ECG): An ECG can help identify abnormal heart rhythms or other electrical problems that may contribute to heart failure.
- Chest X-ray: Chest x-rays help assess lung congestion and look for other causes of dyspnea.
- Other Blood Tests: Additional blood tests, such as serum sodium, blood urea nitrogen, white blood cell count, hemoglobin, and red cell distribution width, may be used to assess the overall health status and to rule out other possible causes for symptoms.
- Specific situations: In some situations, such as when heart failure is secondary to causes upstream from the left ventricle (e.g. mitral stenosis or acute mitral regurgitation), BNP levels may be lower than expected. Furthermore, in patients with conditions like pericardial constriction or flash pulmonary edema, BNP levels are often lower than expected.
C. Key Considerations for BNP Testing
Here’s a summary of the most important limitations and considerations for BNP testing:
- Not a Standalone Test: BNP tests are not definitive and should always be interpreted in the context of a patient’s overall clinical picture.
- False Positives and Negatives: Various factors can lead to false-positive (high BNP in the absence of heart failure) or false-negative (normal BNP despite heart failure) results. These factors must be carefully considered.
- Individual Variability: BNP levels can vary widely among patients with similar heart conditions, requiring individualised interpretation. Tracking an individual patient’s BNP trajectory is more useful than looking at a single result.
- Context Matters: The clinical context, including symptoms, medical history, and other test results, is essential when interpreting BNP results.
- Use Cut-off Values with Caution: While cut-off values help to identify possible heart failure cases, the specific cutoffs should be used with consideration of the patient’s age, sex, kidney function, and other medical conditions. In acute dyspnea, a BNP cut-off concentration of 100 pg/mL provides an excellent negative predictive value (NPV) to exclude heart failure, while higher values (>400 pg/mL) deliver excellent positive predictive value (PPV).
- Serial Measurements: When monitoring treatment, trends in BNP levels over time are usually more important than single measurements. A change of 25-30% or more from a stable level suggests a change in clinical state.
D. Implications for Clinical Practice
- Avoid Over-reliance: Do not rely solely on BNP test results for diagnosis or treatment decisions.
- Individualised Interpretation: Interpret BNP results considering the patient’s unique characteristics, risk factors and symptoms.
- Use BNP in Conjunction with Other Tests: Use BNP and NT-proBNP testing as part of a comprehensive evaluation, which may include an ECG, chest x-ray, echocardiography and other blood tests.
- Consider Serial Testing: Track BNP levels over time to assess treatment effectiveness and disease progression.
- Consult Experts: Consult cardiologists or other healthcare professionals with experience in heart failure management for complex cases.
IX. The Final Word on BNP Testing
B-type natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP) tests are powerful tools in the fight against heart failure. They help us understand how the heart is working, but they aren’t the whole picture. It’s important to know both what these tests do well, and where their limitations lie.
A. What BNP Testing Does Well
- Helps diagnose heart failure: BNP and NT-proBNP tests are useful for identifying heart failure, especially when patients have symptoms such as breathlessness.
- Assesses risk: These tests can help doctors figure out which patients are at a higher risk of problems like hospitalisation or death.
- Monitors treatment: BNP levels can be tracked over time to see if treatments are working and how the disease is progressing. In some conditions like adult congenital heart disease (ACHD), they are particularly useful for assessing risk.
B. Understanding the Limitations
- Not a perfect test: BNP levels can be affected by things other than heart failure, such as age, sex, obesity, and kidney problems.
- Results vary: A single BNP test isn’t always enough to make big decisions. Doctors need to look at the full clinical picture, including a patient’s history and other test results.
- False results are possible: It’s important to know that sometimes the tests can give a false positive or false negative result.
C. A Team Approach to Heart Health
- More than one test: It is important to combine BNP results with other tests, such as echocardiograms, ECGs, and chest X-rays. Sometimes more blood tests are needed to make a clear diagnosis.
- Clinical Judgement: Doctors use their clinical judgement to assess the results of the tests within the wider context of the patient’s health.
- Use in Emergency Settings: Even in emergency settings, where rapid BNP testing can be helpful, it should be be used in conjunction with a complete assessment of the patient.
D. Future of BNP Testing
- New Research: Scientists are always working to better understand BNP and how it can be used. They’re looking at new ways to test BNP and how it can help with other conditions.
- Point-of-Care Testing: There is growing interest in making BNP tests easier and more accessible.
- Personalised Medicine: Combining BNP results with other biomarkers will likely improve risk assessment in the future.
E. What You Need to Know
- One test may not be enough: A single BNP test might not give you all the answers, and further testing may be needed.
- Ask questions: Patients should talk to their doctor about any concerns they have about their heart health.
- Understanding your results: It’s vital that patients understand what their results mean, and what their next steps might be.
F. Key Takeaway
BNP testing is a valuable part of modern medicine, but it’s not a stand-alone answer. It should be used as part of a bigger picture of a patient’s health. With continued research and careful application, BNP tests will continue to improve how we diagnose and manage heart failure.
X. References:
- Fonarow, G. C., Peacock, W. F., Phillips, C. O., Givertz, M. M., Lopatin, M., & ADHERE Scientific Advisory Committee and Investigators (2007). Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. Journal of the American College of Cardiology, 49(19), 1943–1950.
- Francis, G. S., Felker, G. M., & Tang, W. H. (2016). A Test in Context: Critical Evaluation of Natriuretic Peptide Testing in Heart Failure. Journal of the American College of Cardiology, 67(3), 330–337.
- Taylor, K. S., Verbakel, J. Y., Feakins, B. G., Price, C. P., Perera, R., Bankhead, C., & Plüddemann, A. (2018). Diagnostic accuracy of point-of-care natriuretic peptide testing for chronic heart failure in ambulatory care: systematic review and meta-analysis. BMJ (Clinical research ed.), 361, k1450.
- Yusuke Yumita, Zhuoyuan Xu, Gerhard-Paul Diller, Aleksander Kempny, Isma Rafiq, Claudia Montanaro, Wei Li, Hong Gu, Konstantinos Dimopoulos, Koichiro Niwa, Michael A Gatzoulis, Margarita Brida, B-type natriuretic peptide levels predict long-term mortality in a large cohort of adults with congenital heart disease, European Heart Journal, Volume 45, Issue 23, 14 June 2024, Pages 2066–2075, https://doi.org/10.1093/eurheartj/ehae254
- Bettencourt P. M. (2005). Clinical usefulness of B-type natriuretic peptide measurement: present and future perspectives. Heart (British Cardiac Society), 91(11), 1489–1494.
- Ludwikowska, K. M., Tokarczyk, M., Paleczny, B., Tracewski, P., Szenborn, L., & Kusa, J. (2024). Clinical Significance of B-Type Natriuretic Peptide and N-Terminal Pro-B-Type Natriuretic Peptide in Pediatric Patients: Insights into Their Utility in the Presence or Absence of Pre-Existing Heart Conditions. International Journal of Molecular Sciences, 25(16), 8781.
- Mangla, A., & Gupta, S. (2023). Brain-Type Natriuretic Peptide (BNP). Medscape
- Miyakuni, S., Maeda, D., Matsue, Y., Yoshioka, K., Dotare, T., Sunayama, T., Nabeta, T., Naruse, Y., Kitai, T., Taniguchi, T., Tanaka, H., Okumura, T., Baba, Y., Matsumura, A., & Minamino, T. (2022). The Prognostic Value of B-Type Natriuretic Peptide in Patients With Cardiac Sarcoidosis Without Heart Failure: Insights From ILLUMINATE-CS. Journal of the American Heart Association, 11(24), e025803.
- Maisel, A. S., Krishnaswamy, P., Nowak, R. M., McCord, J., Hollander, J. E., Duc, P., Omland, T., Storrow, A. B., Abraham, W. T., Wu, A. H., Clopton, P., Steg, P. G., Westheim, A., Knudsen, C. W., Perez, A., Kazanegra, R., Herrmann, H. C., McCullough, P. A., & Breathing Not Properly Multinational Study Investigators (2002). Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. The New England journal of medicine, 347(3), 161–167.
- Macheret, F., Boerrigter, G., McKie, P., Costello-Boerrigter, L., Lahr, B., Heublein, D., Sandberg, S., Ikeda, Y., Cataliotti, A., Bailey, K., Rodeheffer, R., & Burnett, J. C., Jr (2011). Pro-B-type natriuretic peptide(1-108) circulates in the general community: plasma determinants and detection of left ventricular dysfunction. Journal of the American College of Cardiology, 57(12), 1386–1395.
- Mueller, C., Laule-Kilian, K., Scholer, A., Nusbaumer, C., Zeller, T., Staub, D., & Perruchoud, A. P. (2005). B-type natriuretic peptide for acute dyspnea in patients with kidney disease: insights from a randomized comparison. Kidney international, 67(1), 278–284.
- Tsutsui, H., Albert, N. M., Coats, A. J. S., Anker, S. D., Bayes-Genis, A., Butler, J., Chioncel, O., Defilippi, C. R., Drazner, M. H., Felker, G. M., Filippatos, G., Fiuzat, M., Ide, T., Januzzi, J. L., Jr, Kinugawa, K., Kuwahara, K., Matsue, Y., Mentz, R. J., Metra, M., Pandey, A., … Yoshimura, M. (2023). Natriuretic peptides: role in the diagnosis and management of heart failure: a scientific statement from the Heart Failure Association of the European Society of Cardiology, Heart Failure Society of America and Japanese Heart Failure Society. European journal of heart failure, 25(5), 616–631.
- Müller, C. (2006). The Use of B-type Natriuretic Peptide in Clinical Practice. European Cardiovascular Disease, 2(1), 1–4.
- Welsh, P., Campbell, R. T., Mooney, L., Kimenai, D. M., Hayward, C., Campbell, A., Porteous, D., Mills, N. L., Lang, N. N., Petrie, M. C., Januzzi, J. L., McMurray, J. J. V., & Sattar, N. (2022). Reference Ranges for NT-proBNP (N-Terminal Pro-B-Type Natriuretic Peptide) and Risk Factors for Higher NT-proBNP Concentrations in a Large General Population Cohort. Circulation. Heart failure, 15(10), e009427.
- York, M. K., Gupta, D. K., Reynolds, C. F., Farber-Eger, E., Wells, Q. S., Bachmann, K. N., Xu, M., Harrell, F. E., Jr, & Wang, T. J. (2018). B-Type Natriuretic Peptide Levels and Mortality in Patients With and Without Heart Failure. Journal of the American College of Cardiology, 71(19), 2079–2088. https://doi.org/10.1016/j.jacc.2018.02.071






There’s a calm wisdom in your words — like listening to someone who has truly taken the time to understand the world.
Getting it nearby, like a big-hearted would should
So, how does Tencent’s AI benchmark work? Maiden, an AI is prearranged a plaster down corporation from a catalogue of fully 1,800 challenges, from construction figures visualisations and царствование завинтившемся возможностей apps to making interactive mini-games.
Post-haste the AI generates the jus civile ‘civil law’, ArtifactsBench gets to work. It automatically builds and runs the edifice in a coffer and sandboxed environment.
To awe how the citation behaves, it captures a series of screenshots on the other side of time. This allows it to intimation in own to the unquestionably that things like animations, design changes after a button click, and other unmistakeable consumer feedback.
In the transcend, it hands to the dregs all this submit – the starting importune, the AI’s pandect, and the screenshots – to a Multimodal LLM (MLLM), to exploit as a judge.
This MLLM referee isn’t no more than giving a inexplicit мнение and a substitute alternatively uses a umbrella, per-task checklist to score the consequence across ten conflicting metrics. Scoring includes functionality, buyer circumstance, and unaffiliated aesthetic quality. This ensures the scoring is clear, in harmonize, and thorough.
The convincing without a hesitation is, does this automated reviewer as a consequence incumbency apropos taste? The results snap it does.
When the rankings from ArtifactsBench were compared to WebDev Arena, the gold-standard menu where utter humans distinguish on the in the most front functioning AI creations, they matched up with a 94.4% consistency. This is a elephantine burgeon from older automated benchmarks, which solely managed harshly 69.4% consistency.
On peak of this, the framework’s judgments showed more than 90% entente with seasoned alive developers.
[url=https://www.artificialintelligence-news.com/]https://www.artificialintelligence-news.com/[/url]
Your writing flows like a calm stream over stones, carrying ideas effortlessly, shaping thought with a quiet, deliberate touch, and leaving a lingering sense of clarity and calm.
**mind vault**
mind vault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
**breathe**
breathe is a plant-powered tincture crafted to promote lung performance and enhance your breathing quality.
Your article helped me a lot, is there any more related content? Thanks!
Your article helped me a lot, is there any more related content? Thanks! https://www.binance.info/lv/register?ref=SMUBFN5I
Giờ hãy cùng tìm hiểu chi tiết hơn về những đặc điểm nổi bật đã giúp 888slots game ghi điểm trong mắt cộng đồng người chơi. TONY12-16
Your point of view caught my eye and was very interesting. Thanks. I have a question for you.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me?
E aí, turma da aposta! A betnacional4 parece ser uma boa opção para quem gosta de apostas esportivas. Tem uma boa variedade de esportes e mercados. Vale a pena dar uma olhada! Clica aqui: betnacional4
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.info/zh-TC/register?ref=DCKLL1YD
888slot có chính sách “sinh nhật vàng”: vào ngày sinh nhật (theo CMND), bạn được tặng 88.000 VNĐ + 10 vòng quay miễn phí – chỉ cần cập nhật thông tin chính chủ. TONY01-06H
888slot thường xuyên tung mã giảm giá, voucher nạp tiền – theo dõi fanpage để không bỏ lỡ cơ hội vàng! TONY01-06H
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
You could certainly see your enthusiasm in the work you write. The world hopes for more passionate writers like you who are not afraid to say how they believe. Always follow your heart.
Howdy! I know this is kind of off topic but I was wondering which blog platform are you using for this website? I’m getting fed up of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be fantastic if you could point me in the direction of a good platform.
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Some truly interesting information, well written and broadly user friendly.
**mitolyn reviews**
Mitolyn is a carefully developed, plant-based formula created to help support metabolic efficiency and encourage healthy, lasting weight management.
**herpafend official**
Herpafend is a natural wellness formula developed for individuals experiencing symptoms related to the herpes simplex virus. It is designed to help reduce the intensity and frequency of flare-ups while supporting the bodys immune defenses.
**prostafense**
ProstAfense is a premium, doctor-crafted supplement formulated to maintain optimal prostate function, enhance urinary performance, and support overall male wellness.
**prodentim reviews**
ProDentim is a distinctive oral-care formula that pairs targeted probiotics with plant-based ingredients to encourage strong teeth, comfortable gums, and reliably fresh breath
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
Thank you for your sharing. I am worried that I lack creative ideas. It is your article that makes me full of hope. Thank you. But, I have a question, can you help me? https://accounts.binance.com/el/register-person?ref=DB40ITMB
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.
I think other website proprietors should take this website as an model, very clean and wonderful user friendly style and design, as well as the content. You are an expert in this topic!
I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article. https://www.binance.com/vi/register?ref=MFN0EVO1
Thanks for sharing. I read many of your blog posts, cool, your blog is very good. https://accounts.binance.com/es-AR/register-person?ref=UT2YTZSU